Theme: Innovations and Modernization of Pulmonary Research and Respiratory Medicine
PULMONOLOGY 2023
The 14th International Conference on Pulmonary and Respiratory Medicine (Pulmonology 2023) will be held by Conference Series on August 21-22, 2023. Pulmonology Conference focuses on the theme of “Innovations and Modernization of Pulmonary Research and Respiratory Medicine”. The Pulmonologist Meeting are honored to host high-profile Keynote Speakers from around the world as well as many concurrent oral and poster presentations, Young Researchers Forum, Delegates to discuss and share on key Respiratory health issues treatment and advances in Pulmonology.
Pulmonology 2023 is one of the Pulmonary and Respiratory Medicine meeting which will be visited by all the prestigious Clinicians and basic, translational, and Clinical researchers from all over the world. This Respiratory Congress will help professionals to learn the latest advances in the rapidly evolving field of Pulmonary Medicine. This Pulmonary Medicine Conference gathers the professionals, registered nurses, advance practice nurses, respiratory therapists, and hospitalists to present and learn latest advances, to discuss their experiences, challenges, and research, meet with the colleagues from around the world, and strike new collaborations. It is truly where health science meets tomorrow’s care. We have dealt with various compelling pulmonary diseases events and Healthcare gatherings and develop incredible relations bringing the researchers and associations together.
The Respiratory Medicine Conference invites pulmonologists and respiratory specialists from around the world to discuss current trends in respiratory screening for diagnosis, treatment, and management. The Pulmonology 2023 is focused on sessions covering nearly all respiratory conditions such as COPD, asthma, allergies, cystic fibrosis, pneumonia, tuberculosis, emphysema, lung cancer, complicated chest infections, Thoracic, pulmonary fibrosis, sleep apnea, lung disease, chronic cough, influenza, mycobacterial infection, pulmonary diseases in children, bronchiectasis, intensive care, etc.
Targeted Audience:
The target audience would be the below professionals, but not limited to:
- Pulmonologists
- Respiratory medicine
- Respiratory physicians
- Tuberculosis Societies
- Respiratory Therapy
- Radiology & Radiotherapy
- Health Care Experts
- Behavioral Science
- Infectious Disease
- Physiotherapy
- Respiratory disease specialists
- Pediatric Pulmonary, Critical Care, and Sleep
- Experts of Respiratory Control Program
- General Medicine & Internal Medicine
- Environmental and Occupational Health
About Organization: -
The world's leading expert in organizing academic, scientific, and business conferences, meetings, symposia, and exhibitions in various vertical and horizontal sectors, including medical, pharmacy, engineering, science, technology, and business to advance scientific research . With the kind assistance and collaboration of our 30,000 editorial board members and more than 1,000 scientific societies, we annually host over 3,000 international events, including more than 1,000 conferences, symposia, and workshops throughout the United States, Europe, the Middle East, and Asia. The DOI generated by CROSSREF is included in special issues of our 700+ international open access journals that publish all conference proceedings.
Benefits: -
- The sponsoring journals for the conference and the conference book proceedings will both publish all approved abstracts.
- Each abstract will be given a Cross Ref DOI number. Possibility to hold a workshop with your team members
- One-on-one meetings with keynote speakers, OCM, and prominent figures to plan the future course of work.
- The chance to lead a session.
- The organizing committee's certification.
- Specific keynote A page will be made to increase the exposure of your scientific study.
- Massive Discounts for Group Registration, among other things.
Target audience: -
- Directors of the Associations for pulmonology
- Researchers/Scientists in pulmonology
- Pulmonologists
- Junior/senior research fellows in the fields of pulmonology, nursing, and health care student.
- Directors of pharmaceutical firms.
Track:1 Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease (COPD) is a form of lung illness that progresses and is characterized by persistent respiratory symptoms and reduced airflow. Breathing difficulties and a cough that may or may not produce mucus are the main symptoms. Despite being incurable, COPD can be prevented and treated.
Emphysema and chronic bronchitis are the two phenotypes of COPD that are most frequently diagnosed.
Track:2 Pneumonia
Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli. Symptoms typically include some combination of productive or dry cough, chest pain, fever, and difficulty breathing. The severity of the condition is variable. It is usually caused by infection with viruses or bacteria, and less commonly by other microorganisms. Identifying the responsible pathogen can be difficult.
Track:3 Pulmonary diseases
A type of disease that affects the lungs and other parts of the respiratory system. Pulmonary diseases may be caused by infection, by smoking tobacco, or by breathing in secondhand tobacco smoke, radon, asbestos, or other forms of air pollution. Pulmonary diseases include asthma, chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, pneumonia, and lung cancer. Also called lung disorder and respiratory disease.
Track:4 Asthma
Asthma is a long-term inflammatory disease of the airways of the lungs. It is characterized by variable and recurring symptoms, reversible airflow obstruction, and easily triggered bronchospasms. Symptoms include episodes of wheezing, coughing, chest tightness, and shortness of breath. These may occur a few times a day or a few times per week. Depending on the person, asthma symptoms may become worse at night or with exercise. Asthma is thought to be caused by a combination of genetic and environmental factors. Environmental factors include exposure to air pollution and allergens.
Track:5 Tuberculosis
Tuberculosis (TB) is an infectious disease usually caused by Mycobacterium tuberculosis (MTB) bacteria. Tuberculosis generally affects the lungs, but it can also affect other parts of the body. Most infections show no symptoms, in which case it is known as latent tuberculosis. Around 10% of latent infections progress to active disease which, if left untreated, kill about half of those affected. Typical symptoms of active TB are chronic cough with blood-containing mucus, fever, night sweats, and weight loss. It was historically referred to as consumption due to the weight loss associated with the disease. Infection of other organs can cause a wide range of symptoms.Tuberculosis is spread from one person to the next through the air when people who have active TB in their lungs cough, spit, speak, or sneeze.
Track 6: Influenza
Influenza, commonly known as "the flu", is an infectious disease caused by influenza viruses. Symptoms range from mild to severe and often include fever, runny nose, sore throat, muscle pain, headache, coughing, and fatigue. These symptoms begin from one to four days after exposure to the virus (typically two days) and last for about 2–8 days. Diarrhea and vomiting can occur, particularly in children. Influenza may progress to pneumonia, which can be caused by the virus or by a subsequent bacterial infection. Other complications of infection include acute respiratory distress syndrome, meningitis, encephalitis, and worsening of pre-existing health problems such as asthma and cardiovascular disease.
Track 7: Lung Cancer
Lung cancer, also known as lung carcinoma (since about 98–99% of all lung cancers are carcinomas), is a malignant lung tumor characterized by uncontrolled cell growth in tissues of the lung.[9] Lung carcinomas derive from transformed, malignant cells that originate as epithelial cells, or from tissues composed of epithelial cells. Other lung cancers, such as the rare sarcomas of the lung, are generated by the malignant transformation of connective tissues (i.e., nerve, fat, muscle, bone), which arise from mesenchymal cells. Lymphomas and melanomas (from lymphoid and melanocyte cell lineages) can also rarely result in lung cancer.
Track 8: Cystic Fibrosis
Cystic fibrosis (CF) is a rare genetic disorder that affects mostly the lungs, but also the pancreas, liver, kidneys, and intestine. Long-term issues include difficulty breathing and coughing up mucus because of frequent lung infections. Other signs and symptoms may include sinus infections, poor growth, fatty stool, clubbing of the fingers and toes, and infertility in most males. Different people may have different degrees of symptoms.
Track 9: Pulmonary fibrosis
Pulmonary fibrosis is a condition in which the lungs become scarred over time. Symptoms include shortness of breath, a dry cough, feeling tired, weight loss, and nail clubbing. Complications may include pulmonary hypertension, respiratory failure, pneumothorax, and lung cancer. Causes include environmental pollution, certain medications, connective tissue diseases, infections, and interstitial lung diseases
Track 10: Pulmonary hypertension
Pulmonary hypertension (PH or PHTN) is a condition of increased blood pressure in the arteries of the lungs. Symptoms include shortness of breath, fainting, tiredness, chest pain, swelling of the legs, and a fast heartbeat. The condition may make it difficult to exercise. Onset is typically gradual. A patient is deemed to have pulmonary hypertension if the pulmonary mean arterial pressure is greater than 25mmHg at rest, or greater than 30mmHg during exercise
Track 11: Treatment for Lung Cancer
Surgery, radiation, chemotherapy, targeted therapy, immunotherapy, and combinations of these treatments are available for treating lung cancer. Scientists now have some encouraging findings for advanced-stage lung cancer, but researchers continue to explore for novel therapy options for all stages of the disease.
Track 12: COVID-19
A new coronavirus called SARS-CoV-2 appeared in 2019, sparking a pandemic over the world. Its condition, COVID-19, has the potential to cause mild to severe respiratory sickness as well as mortality. Fever, coughing, exhaustion, bodily aches, and a loss of taste or smell are just a few of the symptoms that can appear. In the face of this immediate health hazard, VA has put in place a prompt public health response to safeguard and care for Veterans and personnel.
Targeted research initiatives, community engagement with Veterans, screening at VA healthcare institutions, a phased immunization deployment, and policies to safeguard patients admitted to community living facilities are some of the measures the VA has done to reduce COVID-19 spread. Visit the COVID-19 topic page to read about the clinical studies, data analytics, and research collaborations that are being conducted by the VA to develop strategies to prevent and cure the new coronavirus.
Track 13: Emphysema
Emphysema, or pulmonary emphysema, is a lower respiratory tract disease, characterized by air-filled spaces (pneumatosis) in the lungs, that can vary in size and may be very large. The spaces are caused by the breakdown of the walls of the alveoli, and they replace the spongy lung parenchyma. This reduces the total alveolar surface available for gas exchange leading to a reduction in oxygen supply for the blood.
Track 14: Oxygen therapy
Oxygen therapy, also known as supplemental oxygen, is the use of oxygen as medical treatment. Acute indications for therapy include hypoxemia (low blood oxygen levels), carbon monoxide toxicity and cluster headache. It may also be prophylactically given to maintain blood oxygen levels during the induction of anesthesia. Oxygen therapy is often useful in chronic hypoxemia caused by conditions such as severe COPD or cystic fibrosis. Oxygen can be delivered via nasal cannula or face mask, or via high pressure conditions such as in endotracheal intubation or hyperbaric chamber. It can also be given through bypassing the airway, such as in ECMO therapy.
Track 15: Obstructive sleep apnea
Obstructive sleep apnea (OSA) is a situation in which breathing stops involuntarily for a short time at some point in sleep. Usually, air flows smoothly from the mouth and nose to the lungs at any time. In obstructive sleep apnea, normal airflow stops again and again throughout the night. Breathing stops because the airway in the throat is too narrow. Snoring is common in obstructive sleep apnea. Obstructive sleep apnea causes episodes of decreased oxygen delivery to the brain and other parts of the body. Good sleep is poor, which causes drowsiness during the sundial and lack of clarity in the morning. There are several forms of sleep apnea, but OSAS is the most common. Obstructive sleep apnea is much more common in older people and overweight people. Evidence shows that weight loss causes improve symptoms. Sleeping in your again can irritate obstructive sleep apnea. The prognosis for obstructive sleep apnea begins with complete records and physical examinations. Daytime sleepiness and snoring are important clues.
Track 16: Pulmonary Rehabilitation
Pulmonary rehabilitation, also known as respiratory rehabilitation, is an important part of treating and maintaining the health of people with chronic respiratory conditions who persist in symptoms or continue to decline in function despite standard treatment. This is a broad therapeutic concept. The American Thoracic Society and the European Respiratory Society describe it as an evidence-based, interdisciplinary, and comprehensive intervention for patients with chronic respiratory conditions who have symptoms and regularly reduce daily activity. In general, pulmonary rehabilitation refers to the sequence of services that are provided to patients with respiratory disease and their families, usually with the aim of improving the patient's quality of life.
Pulmonary rehabilitation can be completed in a variety of settings, depending on the patient's wishes, and may or may not include pharmacological intervention. Pulmonary rehabilitation is usually tailored to the patient's personality to meet his or her desires. It is an extensive program that can benefit people with lung conditions such as chronic obstructive pulmonary disease (COPD), sarcoidosis, idiopathic pulmonary fibrosis (IPF), and cystic fibrosis, among others. Although the technique is aimed at rehabilitating the victim himself, the family is also involved. The system usually does not start until a scientific examination of the victim has been performed by an authorized physician.
Track 17: Interventional pulmonology
Interventional pulmonology is a subspecialty that uses advanced diagnostic and therapeutic procedures to care for patients with benign and malignant diseases of the lung, airways, and pleura. There has been a rapid proliferation of new pulmonary procedural technologies over the last decade. Common diagnostic applications include endobronchial ultrasound, guided bronchoscopy, and several pleural disease interventions. Endobronchial ultrasound is performed with a specially design flexible bronchoscope and allows safe and accurate sampling of intrathoracic structures through the airway wall under direct visualization. Guided bronchoscopy methods are granting significant improvement in the diagnostic yield of flexible bronchoscopy. Virtual bronchoscopy, radial probe endobronchial ultrasound and electromagnetic navigational bronchoscopy are examples of these methods.
Track 18: Mechanical ventilation
Mechanical ventilation may be defined as a life-support system designed to replace or support normal ventilatory lung function. An individual may require mechanical aid for breathing to augment or replace spontaneous ventilatory efforts to achieve medical stability or to maintain life. This support may be short-term, in the form of rescue breathing or manual ventilation, or long-term, employing more advanced techniques of artificial respiration. The patient eligible for mechanical ventilation may require a tracheostomy tube or endotracheal tube for ventilatory support.
Track 19: Treatments for COPD
Currently no cure for chronic obstructive pulmonary disease (COPD), but treatment can help slow the progression of the condition and control the symptoms.
Medical treatment includes
- Bronchodilators: You inhale these medicines. They help open your airways. Ex: Theophylline
- Corticosteroids: These drugs reduce airway inflammation. You could inhale them or take them as pills.
- Combination inhalers: These inhalers pair steroids with a bronchodilator.
- Antibiotics: Your doctor might prescribe these to fight bacterial infections.
- Roflumilast(Daliresp): This drug stops an enzyme called PDE4. It prevents flare-ups in people whose COPD is linked to chronic bronchitis.
- Flu or pneumonia vaccines : These vaccines lower your risk for respiratory illnesses, including COVID-19.
- Pulmonary rehabilitation: This program includes exercise, disease management, and counseling to help you stay as healthy and active as possible.
- Oxygen therapy : You may need this to reduce shortness of breath, protect your organs, and enhance your quality of life.
Surgery
Surgery is usually only suitable for a small number of people with severe COPD whose symptoms are not controlled with medicine
- Bullectomy – an operation to remove a pocket of air from one of the lungs, allowing the lungs to work better and make breathing more comfortable
- Lung volume reduction surgery – an operation to remove a badly damaged section of lung to allow the healthier parts to work better and make breathing more comfortable
- Lung transplant – an operation to remove and replace a damaged lung with a healthy lung from a donor
Track 20:Idiopathic Pulmonary Fibrosis
The interventional pulmonology market size was valued at US$ 3 Bn in 2020 and is expected to reach US$ 8 billion by 2030, expanding growth at a CAGR of 9.1% from 2021 to 2030.
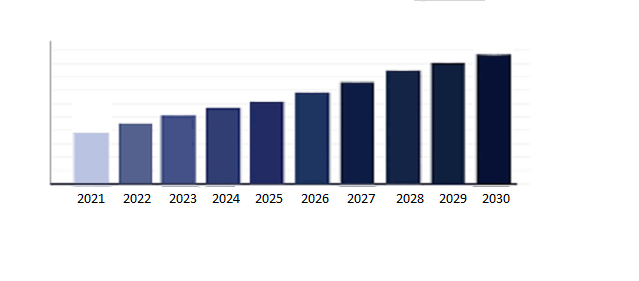
Pulmonary Drug Delivery Systems Market size was valued at USD 43.4 Billion in 2020 and is projected to reach USD 62.9 Billion by 2028, growing at a CAGR of 4.8% from 2021 to 2028.Pulmonary drug delivery systems deliver drugs to the lung for the treatment of diseases of the respiratory tract. This route is preferred broadly due to the non-invasive technique, high blood circulation, large surface area for absorption, and permeability rate. Rise in prevalence of chronic diseases such as bronchitis, tuberculosis, and chronic obstructive pulmonary disease, limitations of traditional treatments for pulmonary delivery, the better penetrability of the drug, minimum dosage requirement, technological advancements, and rise in smoking is expected to drive the market growth. However, regulatory issues related to approval of pulmonary drug delivery systems and high pricing pressures majorly limit the market growth. Factors such as growth opportunities in emerging nations and the rise of online marketing channels offer growth opportunities for the market during the forecast period.
Respiratory Care Devices Market was valued at USD 19.76 Billion in 2019 and is projected to reach USD 39.22 Billion by 2027, growing at a CAGR of 9.65% from 2020 to 2027.
The Global Respiratory Care Devices Market report provides a holistic evaluation of the market for the forecast period. The report comprises various segments as well as an analysis of the trends and factors that are playing a substantial role in the market. These factors: the market dynamics involve the drivers, restraints, opportunities, and challenges through which the impact of these factors in the market is outlined. The drivers and restraints are intrinsic factors whereas opportunities and challenges are extrinsic factors of the market. The Global Respiratory Care Devices Market study provides an outlook on the development of the market in terms of revenue throughout the prognosis period.
The Global Respiratory Care Devices market is expected to grow at a rate of 9.65% because of increasing requirements of respiratory health care. The main reason is the increment in the consumption of tobacco and cigarettes and other major lifestyle changes combined with increase in geriatric population.
Respiratory Care Medical Devices Market size was valued at USD 18.40 Billion in 2022 and is projected to reach USD 40.29 Billion by 2030, growing at a CAGR of 9.1% from 2023 to 2030.
The market is likely to be driven by the rising frequency of respiratory disorders and the aging population around the world in the coming years. In addition, the industry is expected to grow in the next years as urbanization and pollution levels rise. In addition, the market is expected to be fueled in the coming years by the rising prevalence of premature births and changing lifestyle habits. The Global Respiratory Care Medical Devices Market report provides a holistic evaluation of the market. The report offers a comprehensive analysis of key segments, trends, drivers, restraints, competitive landscape, and factors that are playing a substantial role in the market.
PULMONOLOGY 2023
We gratefully express thank all our pleasing speakers, conference attendees, students for making PULMONOLOGY 2022 Conference the best!
The “13th International Conference on Pulmonary & Respiratory Medicine” was held during November 14, 2022, as a Webinar. The generous response was received from the Editorial Board Members of Journals along with scientists, researchers, students, and leaders from various fields of Pulmonology, who made this event a grand success. We are acknowledging with gratitude and support by all the Editorial Board Members of emergency medicine Case Reports for their valuable suggestions for the growth of the Organization.
The conference was initiated with the Honorable presence of the Keynote forum. The heartfelt gratitude to the Organizing Committee Associates, many external experts, company representatives and other eminent personalities who supported the conference by facilitating the discussion forums. We also took the privilege to felicitate the Organizing Committee Members, Editorial Board Members and Media Partners who supported this event.
By the outstanding accomplishment of PULMONOLOGY 2023, it is proud to announce the “14th International Conference on Pulmonary & Respiratory Medicine” to be held during August 21-22 2023, at UAE, Dubai. PULMONOLOGY 2023 has been organized with the intention and the specific intent of promoting the development of new perspectives and ideas for exploiting the high level of Awareness attained by the scientific community in various Pulmonology Services.
Let us meet at @PULMONOLOGY 2023
Conference Highlights
- Chronic obstructive pulmonary disease
- Pneumonia
- Pulmonary diseases
- Asthma
- Tuberculosis
- Influenza
- Lung cancer
- Cystic fibrosis
- Pulmonary fibrosis
- Pulmonary hypertension
- Treatment for Lung Cancer
- COVID-19
- Emphysema
- Oxygen therapy
- Obstructive sleep apnea
- Pulmonary rehabilitation
- Interventional pulmonology
- Mechanical ventilation
- Treatments for COPD
To share your views and research, please click here to register for the Conference.
To Collaborate Scientific Professionals around the World
| Conference Date | August 21-22, 2023 | ||
| Sponsors & Exhibitors |
|
||
| Speaker Opportunity Closed | Day 1 | ||
| Poster Opportunity Closed | Click Here to View | ||
Useful Links
Special Issues
All accepted abstracts will be published in respective Our International Journals.
- Pulmonary & Respiratory Medicine
- Journal of Pulmonology and Respiratory Diseases
- Journal of Pulmonary Medicine
Abstracts will be provided with Digital Object Identifier by








